The Waste Checkbook
Thoughts on the UAE Healthcare Systems
IHI Leadership Alliance recently issued a call for reducing waste in healthcare (IHI, 2019). A report by Bueno, Leo, and Macfie (2019) estimates waste in the US healthcare system at a whopping trillion dollars including non-value added operational and clinical waste as well as costs associated with harm and safety events. The report cites publications supporting the detailed estimates by category. Has waste been systematically quantified in the UAE healthcare systems beyond the effort of individual institutions? The expanding move from fee-for-service model towards implementing the DRG system (Chaudhary, 2019) puts the burden of efficiency on the providers – a situation that hospitals in Abu Dhabi are all too familiar with – and requires aggressive and robust process optimization to sustain operating under the new reimbursement system. Should the UAE healthcare systems further evolve, in a yet to crystallize future, towards the high-value healthcare delivery system advocated by Porter and Lee (2013) with integrated practice units and fully transparent outcomes and cost measures, an infrastructure of granular cost measures at the patient level would be essential. Clarity on what to measure and how to measure has been evolving in the UAE over several years with frameworks like JAWDA in Abu Dhabi and more recently QEYAS in Dubai. However, the scope and granularity of these measurement systems vary greatly and, while several KPIs touch on the operational, none are granular enough to measure costs associated with care delivery processes. For example, if a hospital wishes to understand the cost components of a frequent surgical procedures with questionable profitability, a tool like value stream mapping would be essential along with a controlled process for quantifying and recording cost elements – from surgeons’ time in the OT down to consumables.
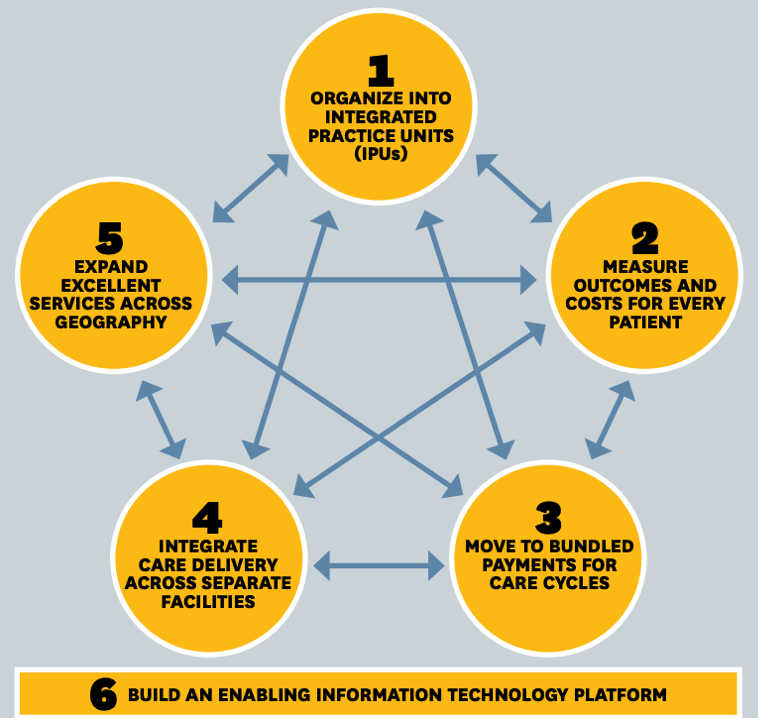
Figure 1: The Value Agenda
The strategic agenda for moving to a high-value health care delivery system has six components. They are interdependent and mutually reinforcing. Progress will be greatest if multiple components are advanced together.

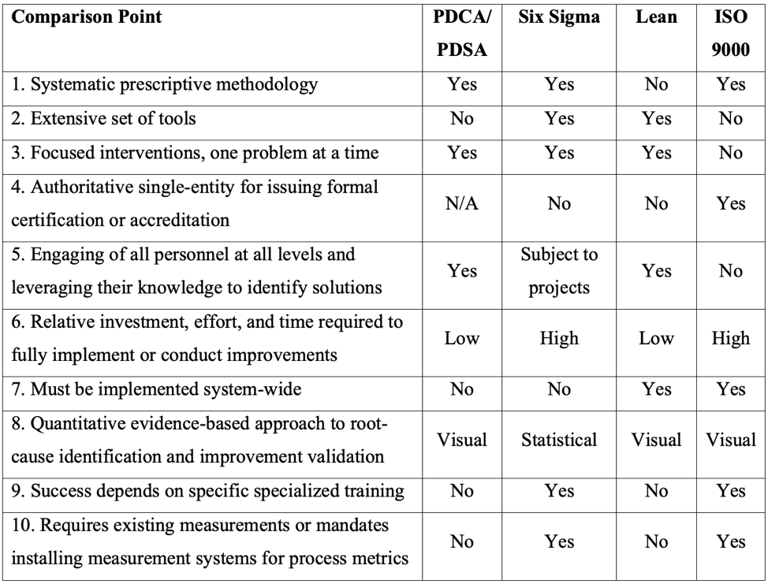
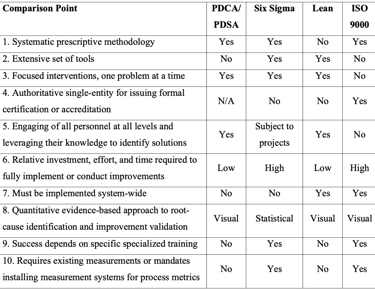
The time is now to start process optimization with robust (Chassin & Loeb, 2011) and proven methods – Lean and Six Sigma – the application of which has been accelerating in healthcare worldwide (Henrique & Filho, 2018) is well documented in several healthcare systems with successes towards both quality and cost (Antony et al, 2018). The good news is, with the wide-spread JCI accreditation of almost all facilities in the country, hospitals are already staffed with quality professionals and many if not most have advanced experience implementing simple quality improvement methods – namely FOCUS-PDCA – but very few have Lean/Six Sigma black belts on board. Few years ago, during my academic studies, I put together this table comparing PDCA, Lean, and Six Sigma. However, away from the method-centric view, the more important questions are: How many hospitals have common systems between the Quality Department and Finance, whereby accountants and quality analysts work together to prioritize areas of cost and methodically attack them with optimization interventions that secure or even improve safety and clinical outcomes while reducing cost? How do leadership teams in hospitals across the UAE view the future and how do they craft their strategies, and where do they see the need to invest in robust process optimization methods?
Source: Porter and Lee (2013)
Table 1:
Comparison of Different Quality Improvement Systems